When online support groups prevail: the information experience of chest/breastfeeders who only express their milk
Fiona M. Jardine.
Introduction. Exclusive pumpers only express their milk and do not feed directly from their breast/chest. Rates of exclusive pumping are increasing, yet information on it is scant. Consequently, exclusive pumpers turn to the internet and online support groups for information and support. This paper examines the information needs of exclusive pumpers, the sources they use, and how useful these sources are. Combined with open-ended responses, this paper provides an insight into exclusive pumpers’ information experiences and its impact on their overall lived experience.
Method. A cross-sectional, self-report, mixed-methods survey was administered online to a convenience sample of current and/or former exclusive pumpers (N = 2, 005).
Analysis. Survey questions pertaining to information experience were analysed quantitatively in SPSS. Inductive thematic analysis of qualitative data was performed in Atlas.ti.
Results. Online sources, particularly online support groups, were the most popular and most useful sources of exclusive pumping information and also provided much-needed support. Having poor information experiences were associated with poorer physical and affective outcomes.
Conclusions. To meet their information needs, exclusive pumpers turn to online support groups and peer-provided information. Healthcare professionals, especially lactation consultants, need to provide improved exclusive pumping information.
DOI: https://doi.org/10.47989/irisic2013
Introduction
Worldwide, the overwhelming majority of parents initiate breastfeeding at birth (Victora et al., 2016); however, many breastfeeders experience difficulties with direct nursing. Because of these difficulties, or simply by choice, some breastfeeders exclusively express/pump their milk; for a more detailed explanation of the use of language in this paper, please see Jardine (2020). Despite the global growth in the numbers of ßexclusive pumpers (Felice and Rasmussen, 2015) and the importance of maximising breastfeeding rates (Bartick and Reinhold, 2010), research on this phenomenon is scant. Examination of exclusive pumpers’ experience of—and outcomes resulting from—information, education and support is all but non-existent. In one exception, the Breastfeeding Without Nursing study collected qualitative and quantitative, cross-sectional data from over 2,000 exclusive pumpers so as to investigate their lived experiences. While study data pertain to a wide range of topics, this paper focuses on exclusive pumpers’ information experience, that is, ‘the complex, holistic nature of people’s engagement with information in real-world contexts’ (Bruce et al., 2014a, p. 4). This paper examines exclusive pumpers’ information needs, seeking behaviour, and use (collectively, information behaviour), information sources and quality, and the effect information has (or not) on lived experience, integrating participants’ ‘thoughts, feelings, senses, and actions; as well as their social and cultural influences’ (Bruce et al., 2014b, p. 316). I do not specifically define the concept of information, but rather believe that we know it when we see it (for more, see Case and Given, 2016). Experience follows von Glasersfeld and Ackermann’s (2011) Erlebnis, as characterised by Savolainen (2019): ‘a person’s experience as lived through: the undergoing of some noticeable event, as apprehended through the senses or mind, affecting him or her here and now’ (p. 9). Given that the Breastfeeding Without Nursing study used a retrospective design, experiences reported by participants were obviously impactful enough to be reportable after the fact.
An examination of information that considers the rich and intricate experiences of exclusive pumpers holistically is vital, for reasons Bruce et al. (2014a) explain:
Attending to information experience opens windows onto people in their informational worlds, revealing their concerns, needs and interests. Understanding people’s information experience has importance for developing or enhancing environments, systems and services that are responsive to and supportive of that experience. (p. 11).
Investigating the lived experiences of exclusive pumpers—as this Breastfeeding Without Nursing study begins to do—is essential to optimally enhance environments, systems, and services for this population, as well as to create evidence-based change to breastfeeding policy, education, and practice more generally.
Given the paucity of research on exclusive pumping, the overall goal of this paper is ‘to explore what is experienced as information and how it is experienced, how information is present or appears, and its role and influence’ (Bruce et al., 2014a, p. 5) among this population. Research questions addressed by this paper include:
- What types of information do exclusive pumpers need?
- What information sources do they use?
- How does information experience contribute to lived experience?
- What barriers affect their information experience?
After briefly describing the importance of breastfeeding, the Breastfeeding Without Nursing study’s research methods are outlined. In order to provide a richer and more contextual discussion of my findings, I review existing breastfeeding and exclusive pumping literature and present results and discussion by topic in the following order: information needs, information seeking, timing of receiving information, information sources, information outcomes, and information barriers. The conclusion identifies overarching concepts and suggests directions for future work.
Background
Human milk is more than just calorific sustenance for infants: it contains a complex and ever-changing combination of proteins, fats, carbohydrates, amino acids, antibodies, white cells, and beneficial bacteria. In their authoritative and expansive systematic review and meta-analysis, Victora et al. (2016) found that breastfeeding has health benefits for both children (e.g., reduced infectious disease mortality, serious diarrhoea, gastrointestinal infections, dental malocclusions, ear infections, and allergic rhinitis) and breastfeeders (e.g., cardiovascular disease, breast cancer, ovarian cancer, and type 2 diabetes). While the long-term benefits of breastfeeding full-term, healthy infants in high-income countries have been questioned (see, for example, Colen and Ramey, 2014), the fact remains that parents—especially those who identify as mothers—see breastfeeding as central to a mothering role (Hauck and Irurita, 2003) and ‘the most natural thing in the world’ (Williamson et al., 2012, p. 434).
However, the majority of breastfeeders do not breastfeed for as long as they wish, often due to a variety of breastfeeding problems. When breastfeeding is challenging, parents feel guilt, a sense of failure and shame (Dennis and McQueen, 2007; Mozingo et al., 2000), as well as inadequacy and isolation (Hegney et al., 2008; Thomson et al., 2015). Caregivers often mourn the loss of the nursing relationship they imagined themselves having. Literature describes the emotions felt as a result of being unable to fulfil breastfeeding goals as: guilt, failure, and shame (Dennis and McQueen, 2007; Mozingo et al., 2000; Thomson et al., 2015); sadness, grief, and trauma (Brown, 2019; Labbok, 2008); inadequacy and isolation (Hegney et al., 2008; Thomson et al., 2015); and anger and perceived judgment and condemnation (Angell, 2017; Lee, 2008; Thomson et al., 2015). Thus, setting aside debates over the objective benefits of breastfeeding, it is essential to optimise breastfeeding support—practical, informational, and emotional—so that those who want to breastfeed have the best possible chance to fulfil their goals.
Although nursing is considered the premier form of breastfeeding (American Academy of Pediatrics, 2012; World Health Organization, 2003), exclusive pumping provides an alternative for those who cannot or do not want to nurse, while retaining most of the benefits of feeding human milk. Exclusive pumpers do not nurse due to a variety of reasons, including failure to latch, infant inability to efficiently suck, a need or desire to monitor intake, having an infant in the neonatal intensive care unit, and/or an actual or perceived low milk supply (Jardine, 2018). There is a small number of breastfeeders who simply choose to exclusively pump (Jardine, 2018).
Methods
Design
A cross-sectional, self-report Qualtrics (www.qualtrics.com) survey was administered in English between 7 March 2017 and 6 March 2018. The survey consisted of 170 open and closed questions, utilising matrix tables, Likert scale-type questions, sliders, and open text boxes where appropriate, although no participant answered every question as survey routing depended on participants’ individual experiences. On average, participants spent 42 minutes filling out the initial survey.
Participants accessed and completed the survey through a URL accessible on any web-enabled device; consent was obtained through the first survey question and compliance with recruitment criteria (current and/or former exclusive pumpers, aged 18 and up) was confirmed in question two. Answering no to either question one or two terminated data collection. Survey routing and categories of questions are shown in Figure 1. Study protocols were reviewed and approved by the Institutional Review Board at the author’s university.
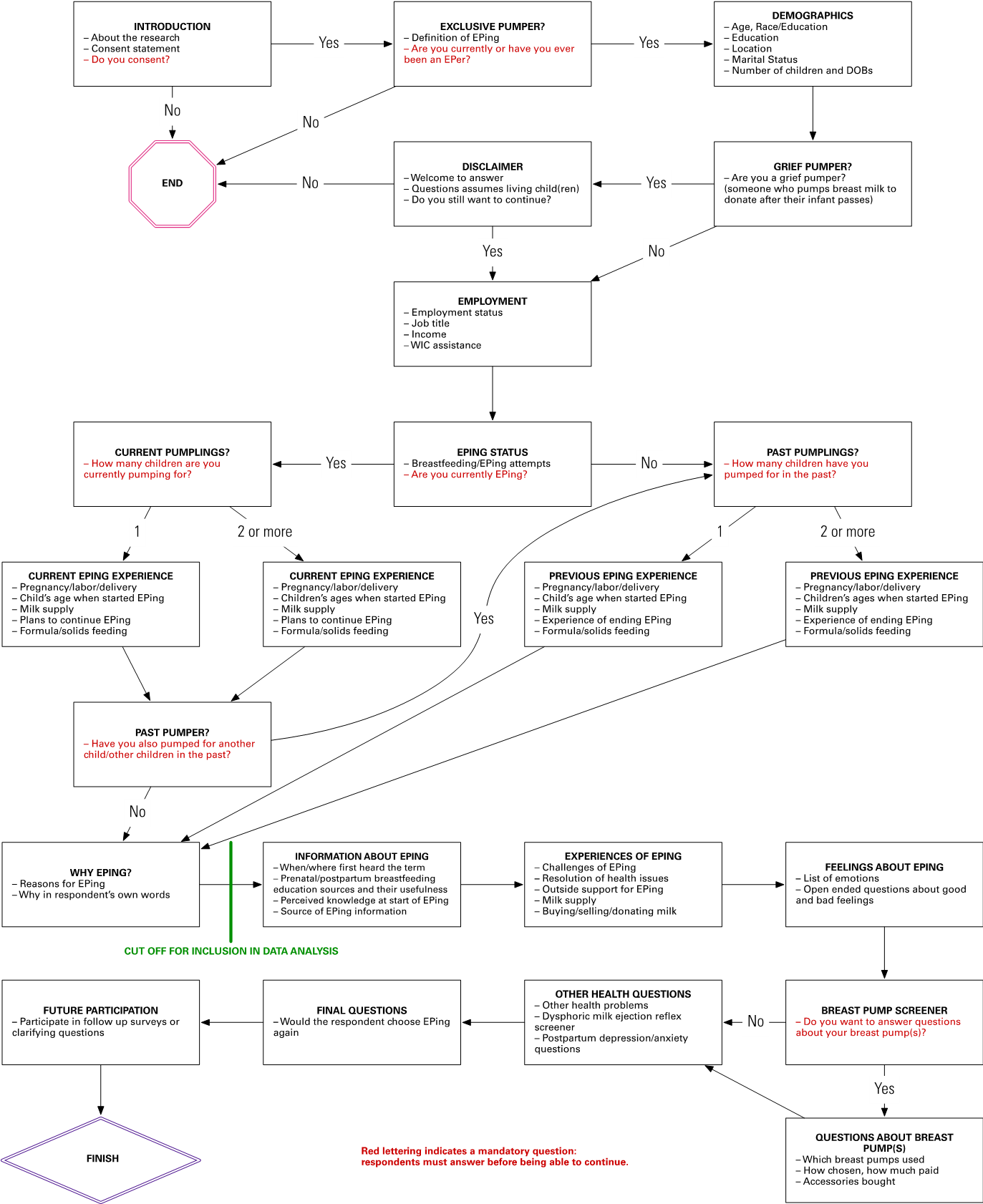
Figure 1. Survey routing and categories included in each section
Sample
A convenience sample was recruited through online support groups and an email newsletter; additional participants were reached through snowball sampling. Of the 2,403 participants who started the survey, 2,005 (83.4%) achieved the data analysis inclusion threshold of 75% survey completion (see Figure 1). Detailed demographics of participants are shown in Table 1. People of colour is used to denote participants who do not identify as White non-Hispanic/Latinx (Moses, 2016).
| Category | N | % |
|---|---|---|
| Year of Birth | ||
| Before 1970 | 4 | 0.2% |
| 1970–1974 | 17 | 0.8% |
| 1975–1979 | 170 | 8.5% |
| 1980–1984 | 552 | 27.5% |
| 1985–1989 | 824 | 41.1% |
| 1990–1994 | 353 | 17.6% |
| 1995–1999 | 61 | 3.0% |
| Missing/Prefer not to answer | 24 | 1.2% |
| Race/Ethnicitya | ||
| Whiteb | 1,665 | 83.0% |
| White Hispanic/Latinx | 129 | 6.4% |
| Asianb | 99 | 4.9% |
| Mixed raceb,c | 36 | 1.8% |
| Black/African-Americanb | 5 | 0.2% |
| American Indian/Alaska Nativeb | 5 | 0.2% |
| Native Hawaiian/Pacific Islander | 0 | 0.0% |
| Non-White Hispanic/Latinx | 37 | 1.8% |
| Missing/Prefer not to answer | 19 | 0.9% |
| People of colour | 311 | 15.5% |
| Residence | ||
| USA | 1,694 | 84.5% |
| Canada | 89 | 4.4% |
| Australia and New Zealand | 55 | 2.7% |
| UK | 48 | 2.4% |
| Other Europed | 15 | 0.7% |
| Asia (not including the Middle East)e | 48 | 2.4% |
| Middle Eastf | 5 | 0.2% |
| Africag | 3 | 0.1% |
| South Americah | 3 | 0.1% |
| Missing/Prefer not to answer | 45 | 2.2% |
| Education | ||
| Some high school | 13 | 0.6% |
| High school or equivalent | 106 | 5.3% |
| Some college/university | 350 | 17.5% |
| Associate (2-year) degree | 196 | 9.8% |
| Bachelor’s degree | 608 | 30.3% |
| Some graduate | 128 | 6.4% |
| Master’s degree | 452 | 22.5% |
| PhD/JD/MD etc. | 118 | 5.9% |
| Trade qualification | 29 | 1.4% |
| Missing/Prefer not to answer | 5 | 0.2% |
| Household Incomei | ||
| Less than 10,000 | 31 | 1.5% |
| 10,000–29,999 | 115 | 5.7% |
| 30,000–49,999 | 234 | 11.7% |
| 50,000–69,999 | 323 | 16.1% |
| 70,000–99,999 | 481 | 24.0% |
| 100,000–149,999 | 419 | 20.9% |
| Greater than 150,000 | 274 | 13.7% |
| Missing/Prefer not to answer | 128 | 6.4% |
| Employment Statusa | ||
| Full time | 1109 | 55.3% |
| Part time | 358 | 17.9% |
| Self-employed | 114 | 5.7% |
| Student | 115 | 5.7% |
| Stay at home parent | 544 | 27.1% |
| Unemployed | 28 | 1.4% |
| Disabled | 11 | 0.5% |
| Retired | 0 | 0.0% |
| On maternity leave | 277 | 13.8% |
| Missing/Prefer not to answer | 3 | 0.1% |
| Relationship Status | ||
| Married | 1,692 | 84.4% |
| In a committed relationship | 272 | 13.6% |
| Single | 26 | 1.3% |
| Separated/Divorced | 13 | 0.6% |
| Widowed | 1 | 0.0% |
| Missing/Prefer not to answer | 1 | 0.0% |
| Number of Children Birthed | ||
| 1 | 1,289 | 64.3% |
| 2 | 532 | 26.5% |
| 3 | 129 | 6.4% |
| 4 | 34 | 1.7% |
| More than 5 | 19 | 0.9% |
| Missing/Prefer not to answer | 2 | 0.1% |
|
Notes: a Participants could select multiple options. b Non-Hispanic/Latinx. c This is an aggregate of participants who selected two or more answers. d Finland (4; 0.2%); Ireland (3; 0.2%); Germany (2; 0.1%); Denmark (2; 0.1%); Belgium (1; 0.1%); France (1; 0.1%); Greece (1; 0.1%); Sweden (1; 0.1%). e Singapore (24; 1.2%); Malaysia (10; 0.5%); India (6; 0.3%); Philippines (4; 0.2%); Hong Kong (3; 0.2); Indonesia (1; 0.1%). f United Arab Emirates (2; 0.1%); Israel (1; 0.1%); Kuwait (1; 0.1%); Qatar (1; 0.1%). g South Africa (2; 0.1%); Mauritius (1; 0.1%). h Peru (2; 0.1%); Guatemala (1; 0.1%). i US dollars. |
||
Data analysis
Qualifying survey responses were downloaded from Qualtrics and data were cleaned in Microsoft Excel (Version 16.33). Quantitative data were then analysed in SPSS (Version 25.0.0.2). Non-parametric tests were performed as Shapiro-Wilk tests demonstrated data to be non-normally distributed; statistical significance was determined when p < .05. Since only questions required for correct survey routing were mandatory, calculations (outside of Table 1) are based on the number of participants answering that question.
As illustrated in Table 1, participants were predominantly resident in the United States, White, well-educated, and with higher levels of household income. This is likely due to the avenues of recruitment (English-speaking online support groups), but also related to the demographics of breastfeeders in general (e.g., Li et al., 2019). Furthermore, a number of studies have found that breastfeeders who express milk have more education, higher household incomes and are more likely to be employed (Bai et al., 2017; Hornbeak et al., 2010; Labiner-Wolfe et al., 2008; Sutter et al., 2018). Although data on the rates of exclusive pumping are not routinely collected, having discussed this topic with international colleagues within breastfeeding and lactation research, it is consistently believed that the United States has a far greater proportion of exclusive pumpers than other English-speaking countries. When quantitative statistical tests were performed, United States participants were compared with non-United States participants and any differences between these groups are noted.
Given that participants were predominantly recruited from online groups, quantitative data only provides a superficial view of information experience—the most popular information source for many topics was, unsurprisingly, online support groups. Therefore, participants’ narrative responses—to all open-ended questions, not just those pertaining to information—are essential to provide valuable insight into the interaction between their experience of information and the context of that experience. These qualitative data were coded in Atlas.ti (Version 8.4.4; atlasti.com) using inductive thematic analysis per Braun and Clarke (2006).
Coding the entirety of the qualitative dataset was not possible (it amounts to over 500,000 words) therefore 30% of responses were randomly chosen to be coded; it was clear that a saturation of codes had been achieved by this threshold (Saunders et al., 2018). Themes were identified at a semantic level (i.e., based on the explicit/surface meanings in participants’ narratives). By analysing thematic patterns within each qualitative survey question and how themes corresponded with other survey data and existing literature, ‘the significance of the patterns and their broader meanings and implications’ (Braun and Clarke, 2006, p. 84) could be explored. It is through this analysis that participants’ information experiences are revealed.
Results and Discussion
Information needs
Scores of studies demonstrate that breastfeeding information has to be clear, concise, consistent, and correct (e.g., Brown, 2016; Clifford and McIntyre, 2008; Graffy and Taylor, 2005; Smale et al., 2006; Spear, 2004; Spiro, 2016; Williamson et al., 2012). Brown (2016) found a need for breastfeeding information that stressed benefits other than infant health (e.g., convenience, cost, and closeness), employed less of an all-or-nothing approach, and included information about both the positive and negative aspects of breastfeeding. Advice needs to be realistic: idealised expectations of breastfeeding leave parents ‘feeling unprepared when they encountered pain, problems and relentlessness of early infant feeding, leading to feelings of guilt and inadequacy over their feeding decisions’ (Fox et al., 2015, p. 147).
Dietrich Leurer and Misskey (2015) identified milk expression as an information gap among the breastfeeders they studied, detailing specific needs as pumping, milk storage, and maintenance of supply with milk expression. In their analysis of milk expression and breast pumping posts from 2014 in an online forum, Yamada et al. (2016) found that four main themes (i.e., information needs) emerged from the posts: ‘choosing and purchasing pumps; storing and preparing pumped human milk; strategies for and difficulties with pumping and integrating pumping into work; [and] stopping pumping’ (p. 4). In Dietrich Leurer et al.’s (2019) study of non-exclusive pumpers, ‘participants sought timely, practical, and factual information, although psychological support was also important’ (p. 6). Participants wanted information about how to pump, frequency and duration of pumping, milk storage, pumps and accessories, and milk supply.
- In response to ‘When you decided to EP/found yourself EPing, how important was information about the following topics?’, Breastfeeding Without Nursing study participants rated the importance of information about a variety of exclusive pumping topics on a Likert-type scale, as illustrated in Table 2. Reflecting Dietrich Leurer et al. (2019), basic logistical topics, such as when and how often to pump and feed, are of high importance. Since most (84.5%; 1,996/2,361) exclusive pumping journeys were started within the first month of their child(ren)’s life, how to wean or decrease supply is low on the list of priorities. Interestingly, despite many parents having to feed formula, the importance of this information was also low—perhaps because participants had already received formula-feeding knowledge before starting to exclusively pump.
| Category | Mean importance scorea | More important tob |
|---|---|---|
| How often to pump | 1.9 |
• People of colour* • U.S. residents* |
| How to maintain supply | 1.7 |
• Participants who exclusively pumped for their second child(ren) or later* • Participants with lower educational attainment* • Non-U.S. residents* |
| How long each pumping session should be | 1.7 | • Participants with higher household income*** |
| How to avoid discomfort/increase comfort | 1.7 | · U.S. residents* |
| Flangec sizing | 1.7 | · U.S. residents*** |
| Breast pump operation/settings | 1.6 | |
| How to store/heat up milk | 1.6 |
• People of colour** • Participants with lower educational attainment*** • Participants with lower household incomes** |
| How to increase supply | 1.6 |
• People of colour* • Non-U.S. residents* |
| How much to feed | 1.2 | • Participants exclusively pumping for their first child(ren)** |
| How often to feed | 1.2 |
• Participants exclusively pumping for their first child(ren)** • U.S. residents* |
| How much milk to pump | 1.2 | |
| How to pump while out of the house | 1.1 |
• People of colour* • Participants with lower household incomes* |
| How to look after child/children while pumping | 0.9 |
• People of colour* • Participants with lower educational attainment* • Participants with lower household incomes** |
| Choice of feeding bottles/nipples | 0.6 | • People of colour* |
| How to explain exclusive pumping to others | 0.3 |
• Participants with lower educational attainment*** • Participants with lower household incomes*** • Non-U.S. residents* |
| How to wean off the breast pump | 0.2 | • Participants with lower educational attainment** |
| How to supplement with formula | 0.1 |
• Participants exclusively pumping for their first child(ren)** • People of colour*** |
| How to get back to the breast | 0.1 |
• Participants who exclusively pumped for their second child(ren) or later** • People of colour*** • Non-U.S. residents*** |
| How to decrease supply | –0.2 |
• Participants with lower educational attainment*** • Participants with lower household incomes** |
|
Notes: *p ≤ .05, **p ≤ .01, *** p ≤ .001 a Likert-type answers were coded as follows: • Not at all important = –2 • Somewhat not important = –1 • Neutral = 0 • Somewhat important = 1 • Very important = 2 b Mann-Whitney U tests (when participants were divided into two groups) and Kruskal-Wallis H tests (when participants were divided into three or more groups) revealed scores reported by these groups were significantly higher or lower than those not in these groups. c This is the funnel-shaped shield that fits over the nipple and areola. |
||
Some types of exclusive pumping information were more important to different groups. It is worth noting that there were was no correlation between race/ethnicity (white non-Hispanic vs. people of colour) and level of education, Mann-Whitney z = –0.719, p = .472, but lower income was correlated with both being a person of colour, z = –2.461, p = .014, and with lower educational attainment, Somers’ d = .393, p < .001. Patterns in these findings reflect those of previous studies on breastfeeding in general: for example, those with lower household incomes are less likely to have as much parental leave following childbirth (Horowitz et al., 2017) and therefore information on how to pump outside the house and store and heat up milk might be a more immediate need. Similarly, these breastfeeders may not have as much social and financial support to be able to find others to look after their child while they pump. Previous research reveals higher formula-feeding rates in communities of colour (Li et al., 2019); therefore, it may not be surprising that these study participants considered information about bottles and nipples and how to supplement with formula more important.
Furthermore, those exclusively pumping for first-born children, logically, have less infant feeding experience and therefore value information pertaining to logistical questions, such as how much and how often to feed as well as how to supplement with formula. The types of information that were more important to participants who exclusively pumped for their second child or later may be informed by their previous breastfeeding experiences—experiences they may aspire to (e.g., getting ‘back to the breast’) or avoid experiencing again (e.g., not maintaining supply). How to explain exclusive pumping and getting back to the breast may be more important to those outside of the United States because pumping is less common in non-United States countries.
Information seeking
Information seeking usually, though not always, follows having an information need, whether articulated as such or not and can be defined as ‘the purposive seeking for information as a consequence of a need to satisfy some goal’ (Wilson, 2000, p. 49). However, information is also gathered through serendipitous discovery (Erdelez et al., 2016). The antitheses of information seeking include information avoidance and blunting (avoiding and seeking distraction) (Case et al., 2005; Rood et al., 2015).
With the ever-increasing medicalisation of pregnancy, childbirth, and parenting (Kukla and Wayne, 2016) and the association between breastfeeding and health outcomes, seeking information about infant feeding is undeniably a form of health information seeking behaviour. Based on her study of Canadian women pregnant with twins, McKenzie (2003) developed a two-dimensional model of health information seeking behaviour with four different modes of information seeking behaviour: active seeking, active scanning, non-directed monitoring, and obtaining information by proxy. When individuals connect and interact with information sources, information seeking behaviour include: actively looking for an information source about a specific topic and asking a pre-planned question (active seeking); identifying and browsing a likely information source and actively reading/listening (active scanning); unexpected serendipitous encounters and observing/overhearing in unexpected places or with acquaintances (non-directed monitoring); and being identified as having an information need and being told (obtaining information by proxy) (paraphrased from McKenzie, 2003, p. 26). This model of information seeking is well-suited to breastfeeding and exclusive pumping information seeking, particularly given that it was derived from a study of pregnant people’s everyday-life information seeking—that is, ‘the ways in which people access and use various information sources to meet information needs in areas such as health, consumption, and leisure’ (Savolainen, 2009, p. 1780).
The Breastfeeding Without Nursing study was not designed to identify specific information seeking behaviours in the way defined by McKenzie (2003): as demonstrated by other studies of everyday-life information seeking (e.g., Erdelez, 1997; McKenzie, 2003; Williamson, 1998; Zimmerman and Wieder, 1977), retrospective in-depth, in-person interviews and/or diary keeping are more appropriate methodologies to collect these kinds of data. Nevertheless, wherever possible in the paragraphs that follow, Breastfeeding Without Nursing study participants’ information seeking behaviour is connected to McKenzie’s (2003) model.
Study participants’ answers to What unanswered questions do you still have about EPing? and ongoing participation in online EPing support groups suggest non-directed monitoring, but also continuous, cumulative, and looped information seeking behaviour. For example, a few participants mentioned non-directed monitoring that led to serendipitous information encounters:
I’m always finding out stuff, unexpectedly.
So many different questions, I have asked the group or am watching the group [to get the answers].
Other participants described ongoing active information seeking. For example:
I learned about EPing though an internet search. … I am constantly googling and searching for information, tips, and just common experiences of other EPers.
Continuous monitoring of or active seeking for information sources leads to serendipitous discoveries of relevant and useful information, aligning with Bruce’s (2005) personal anticipated information need theory. That is, by monitoring questions and discussions in these groups, study participants ‘acknowledge the usefulness of the information but delay the information use to another time’ (Bruce, 2005, sec. Proposition 1). One participant aptly summed this up:
I don’t have any questions today but you never know what will come up tomorrow that will trigger some insight from the EP [exclusive pumping] tribe.
Timing of information
Spear (2004) highlighted the importance of receiving accurate information about breastfeeding initiation prior to birth, including what could go wrong or what alternative methods might need to be employed. She stressed that ‘explanation about alternative feeding methods for infants who cannot be breastfed initially, familiarization with use of the breast pump, and hand expression of milk prior to delivery may be helpful’ (p. 774), not only practically, but also to prevent idealised and unrealistic expectations of the breastfeeding experience (see also, Fox et al., 2015; Mozingo et al., 2000). Relatedly, the mothers studied by Graffy and Taylor (2005) felt that the information they were given prenatally did not reflect the ‘realities of breastfeeding,’ such as ‘discomfort and the time they might spend feeding, and … common feeding problems’ (p. 181).
- Many Breastfeeding Without Nursing participants wished they had known about exclusive pumping sooner:
Knowing it existed and was so common before I gave birth [would have make exclusive pumping better]. Had I known it was a possibility before, I wouldn’t have had such a hard time when we ‘failed’ at breast feeding. I wish I had known it wasn’t direct nursing or nothing.
Of those participants who EPed for their first child, only 23.3% (386/1,654) had heard of the term exclusive pumping prenatally. Given this, participants were unable to actively seek or scan for information specifically concerning exclusive pumping—participants simply did not know it was a thing. Many participants serendipitously encountered information about exclusive pumping while searching for breastfeeding help more generally; while they were actively seeking or scanning for other information, they stumbled across exclusive pumping. For example:
I stumbled upon the term exclusive pumping while looking for info on Pinterest. I saw there was a Facebook group called Exclusively Pumping Mamas and felt such relief and happiness to know I wasn’t alone. I didn’t realize exclusively pumping was a thing other people did as well.
>I stumbled upon it in research online on the kellymom website. I then explored videos online and eventually found the Facebook support groups.
Exclusive pumpers need substantive information sooner. In responding to the prompt, What would have made exclusive pumping better?, the theme of finding support and information sooner was second only to more and/or better information:
Knowledge. Learning before I had to do would have helped. I had no idea that this was even an option. I had to learn as I went. By 6 months, I finally felt knowledgeable. After 6 months of doing it while feeling clueless.
Unfortunately seeking out prenatal breastfeeding information/education did not particularly help participants to learn about exclusive pumping, as Figure 2 displays. Doing one’s own research and reading, closely followed by a class that included breastfeeding information, were the most popular sources of prenatal breastfeeding education. However, even the source with the highest likelihood of including exclusive pumping in some way—own research/reading—only did so just over half the time.
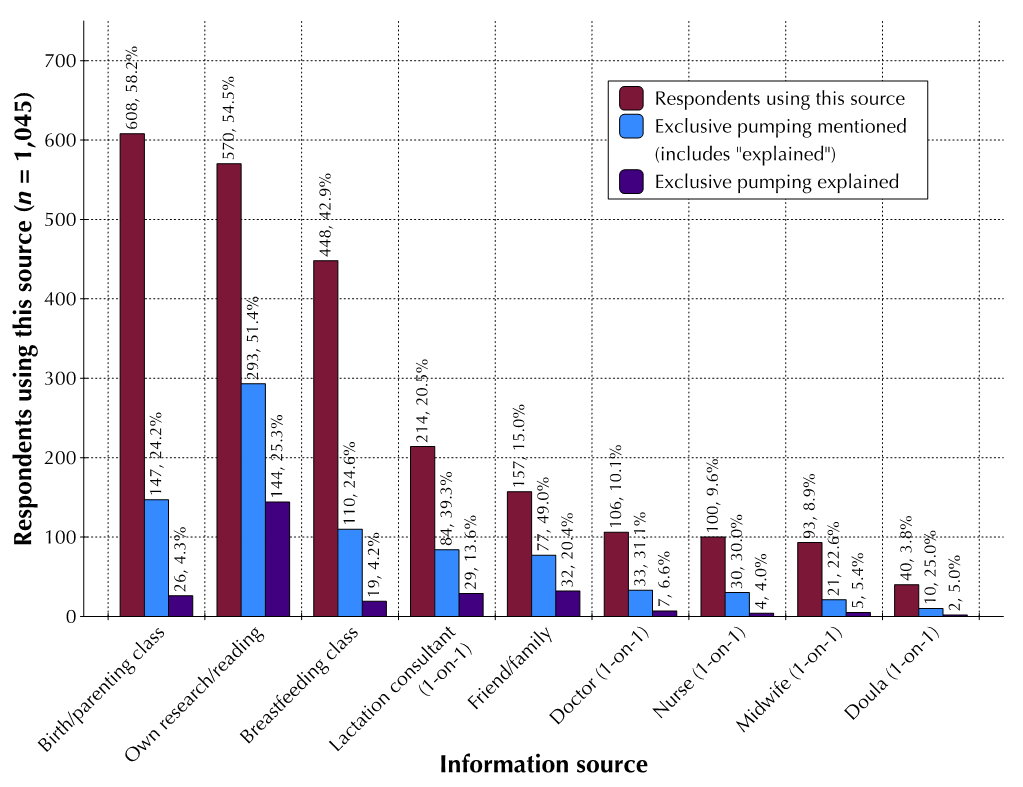
Figure 2. Participants sources of prenatal breastfeeding education, showing the proportion of sources that mentioned or explained exclusive pumping (n = 1,045)
This participant succinctly communicates a typical breastfeeding education experience:
I took a breastfeeding class before giving birth and it was never discussed what to do if baby won’t latch. After baby was born, it would have been nice to have someone who could tell me about exclusively pumping, all the lactation consultants I saw never mentioned it or when I said that’s what I was doing they acted as if it wouldn’t work.
Information sources
Breastfeeders prefer information from sources they perceive to be trustworthy and/or that provide information from lived experience (Loudon et al., 2016; Song et al., 2013), including healthcare providers, family members, and friends (Grimes et al., 2014; Kamali et al., 2018; McDougall and Ecclestone, 2015). Books and other printed materials were found to be among the most useful sources in some studies (e.g., Grimes et al., 2014), while others did not find these sources useful (e.g., McDougall and Ecclestone, 2015). The internet is an important and frequently used source of parenting information (Nolan et al., 2017; Papen, 2013; Sayakhot and Carolan-Olah, 2016). Breastfeeding information sources also include community-based peer groups (e.g., Shakya et al., 2017), the child’s grandmother(s) (e.g., Cox et al., 2017; Karmacharya et al., 2017), and online social networks (Gray, 2013; McKeever and McKeever, 2017), although Asiodu et al. (2015) found that infant feeding information on social media was either not present or not memorable. Bartholomew et al. (2012) found that 44% of the mothers in their study reported more Facebook use after birth, primarily to build and maintain weak-tie connections, not seek information. In contrast, Gray (2013) found that the majority of breastfeeding posts on a variety of online discussion boards sought (79%) or provided (62%) informational support, with another 8% of posts seeking and 9% of posts providing tangible support, respectively. In an analysis of Twitter use by mothers before and after birth, 15% reduced their social media interactions after birth, but what they did tweet displayed ‘a number of changes in emotion expression in a generally negative direction’ (De Choudhury et al., 2013, p. 1440). Nevertheless, Madge and O’Connor (2006) found that the internet increased their participants’ ‘sense of empowerment in the transition to motherhood’ (p. 199), despite the traditional stereotypes of mothering and gender roles.
There are few studies assessing exclusive pumping information sources. According to Rasmussen and Geraghty (2011),
'at present, the lay literature (e.g., magazine articles, Internet postings) remains a major source of information about maternal behavior related to milk expression, and some of these behaviors are of public health concern.' (p. 1356).
However, McInnes et al. (2015) found that milk expression and pumping information on United Kingdom websites was inconsistent, incomplete, and not evidence-based. In contrast to Rasmussen and Geraghty (2011), Sutter et al. (2018) found that 78.3% of their participants (United States women at 6 weeks postpartum) had obtained pumping information from professional sources, whereas over one third (38.9%) had received support on breast pumps and milk expression from their friends and/or relatives.
Most recently, Dietrich Leurer et al. (2019) found that lactation consultants were the most common source of valuable information about pumping, followed by the internet, friends/family, and other mothers, including mother-to-mother online support groups; nurses and physicians ‘did not or were unable to provide the desired expression information’ (p. 6).
Breastfeeding Without Nursing study participants were asked How useful were the following sources of information when finding out information about exclusively pumping?. Table 3 presents the number and proportion of participants who used each source for exclusive pumping information.
| Source | n | % |
|---|---|---|
| Online support groups | 1,721 | 94.4 |
| Websites | 1,569 | 86.1 |
| Lactation consultant | 1,515 | 83.1 |
| Doctor | 1,280 | 70.2 |
| Nurse | 1,254 | 68.8 |
| Friend/family member | 1,204 | 66.0 |
| Books | 939 | 51.5 |
| Leaflets/pamphlets | 751 | 41.2 |
| Journal articles | 741 | 40.6 |
| Midwife | 551 | 30.2 |
| Magazines | 457 | 25.1 |
| Newspapers | 415 | 22.8 |
| Television | 402 | 22.1 |
| Radio | 376 | 20.6 |
| Doula | 252 | 13.8 |
It was unexpected to find approximately one in five respondents had used more traditional information sources, such as newspapers (22.8%; 415/1,823), television (22.1%; 402/1,823), and radio (20.6%; 376/1,823). On a visual inspection of responses by participants who rated these sources (and perhaps magazines as well), they seldom selected not applicable/I did not use this source. Some participants only selected this option for sources presented to them later in the question. It seems likely, therefore, that participants who rated these sources did not utilise this opt-out option appropriately, therefore giving the impression that they had used these sources to find exclusive pumping information when they had not. Unfortunately, excluding responses that never selected the not applicable/I did not use this source response option would not solve this problem, as some participants never selected this option because they left blank those sources they (presumably) did not use; other participants appeared to have realised that there was a not applicable/I did not sue this source option part way through the question, but it would be impossible to discern this with certainty.
Nevertheless, it seems reasonable to assume that the overall findings as to the usefulness of each source of exclusive pumping information, especially as compared to each other, remains valid (i.e., participants would likely not have rated a source they had never used as useful). This data is presented in Figure 3 and illustrates that online support groups, followed by websites, friends/family members, and lactation consultants were perceived to be the most useful sources of information about exclusive pumping.
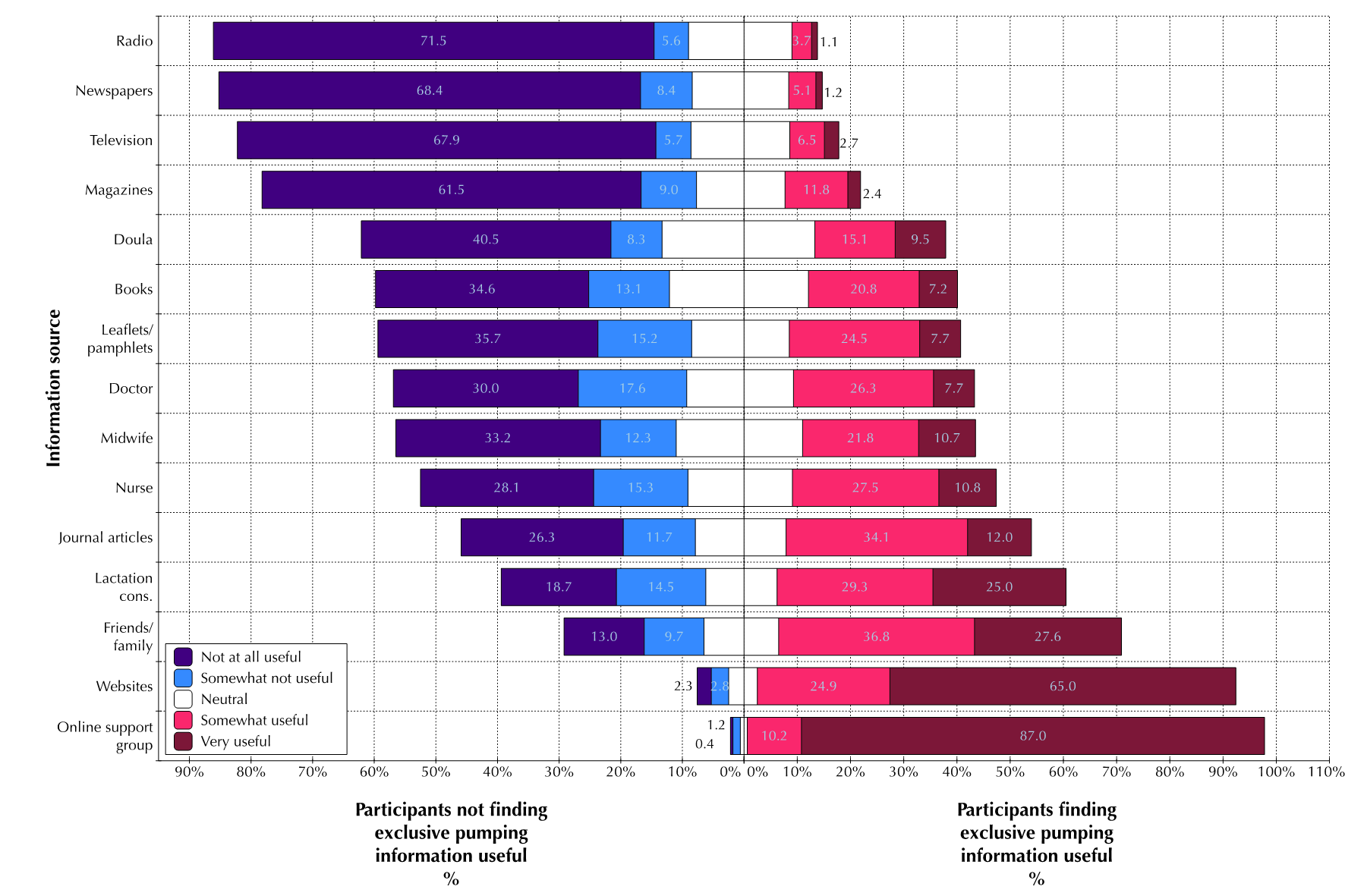
Figure 3. Responses to ‘How useful were the following sources of information when finding out information about exclusively pumping?’ (n = 1,823)
The use of journal articles was also surprisingly high—40.6%—and were rated as the fifth most useful source. Using journal articles did not correlate with education level, race, income level or country of residence. One participant ‘got great info’ from journal articles because of preferring ‘to go to the source whenever possible as I research anything that interests me.’ Another participant used journal articles to supplement their existing knowledge:
After learning more from fellow exclusive pumpers in these [online support] groups, I was able to extend my knowledge by browsing journal articles and identifying the success of certain techniques/methods of increasing supply and other related pumping issues.
Some participants wished there were more journal articles and research on exclusive pumping. For example, one participant,
mostly used online searches and Facebook groups … for answers to my pumping questions. I did not feel good about this - I wanted solid, data-driven answers and these places felt more anecdotal. But I did not find the resources I was looking for.
Another participant wanted ‘more university-conducted research on EP [exclusive pumping] so I could have a more reliable source.’
Despite the myriad of sources used, online support groups and websites were clearly considered the most useful for exclusive pumping information. While this could be influenced by the recruitment method for this study, many participants had sought information offline before finding online support groups. In response to the question, What would have made exclusive pumping worse?, a predominant theme was not having online support and information. Finding an online support group, such as a Facebook group, was a noticeable event that greatly improved participants’ information experiences:
If I hadn’t stumbled onto that Facebook group, I think I would have miserable for a bit longer than I was. I was getting my shit sorted out but that group really was a game changer for me.
Online support groups provided participants with ‘a group of women…to ask loads of questions to’ and participants felt reassured by this, especially if they had had poor information experiences with healthcare provider/lactation consultants:
It’s great knowing there are many other women that have experienced issues I’m just now experiencing so that I can have actual answers not just what doctors are trained to say.
Participants explained in their own words why online support groups were the most useful source for exclusive pumping information:
I learned most about EPing [exclusive pumping] through my own research via websites and on Facebook support groups. I got the most useful answers via the online support groups and I felt the information was useful even if it wasn’t from a medical professional or peer reviewed journal since it was advice about various experiences.
I have learned the majority of my knowledge through Facebook groups. It’s quick and convenient and there are women going through what I’m going through at the same time. It’s not just learned knowledge but experience. I’m am very pleased with the information I’ve gathered so far.
However, other participants were cautious about the information they received through online support groups. One felt that ‘there is a lot of misinformation in some of the Facebook groups’ and another said:
I trust the websites because they are more research based (cite journals, books, studies) & written by nurses/LCs [lactation consultants]. The Facebook page is good for support but I take somethings with a grain of salt because the members are not all health providers.
To combat potentially poor information, one participant stated that they get ‘most of my there [Facebook groups] and then look up things to confirm the accuracy.’ Another has ‘to remember to take everything as opinion, unless I’m reading a research article or something from kellymom [evidence-based breastfeeding website] for instance.’
However, the importance of common experience and sharing knowledge gained through experience cannot be understated. Membership in online support groups became a sociocultural experience for many of the participants—one that helped them improve physical (e.g., increased pumping duration) and affective (e.g., feelings of support) outcomes. Several participants characterised their membership of a Facebook group as being part of a tribe:
I was so lost the first 14 weeks. Once I found the [Facebook] group my whole world changed. I finally found my tribe and recommend it to EVERYONE. I wouldn’t have lasted as long as I did without them.
Likewise, ‘not having the Facebook group to rely on for guidance and assistance from my EP [exclusive pumping] tribe’ and ‘lack of the Tribe’ would have made these two participants’ exclusive pumping journeys worse. A full analysis of the role of online support groups in the lived experiences of Breastfeeding Without Nursing study participants is outside of the scope of this paper.
Breastfeeding information outcomes
Breastfeeding duration is significantly increased when information, advice, and support are provided on an ongoing basis (Fu et al., 2014; Hoyer and Horvat, 2000; Shakya et al., 2017). Although Lumbiganon et al.’s (2016) meta-analysis of 24 studies found no conclusive evidence indicating that prenatal peer counselling, lactation consultation, or formal education increased breastfeeding initiation and duration, providing information and support postpartum does impact breastfeeding outcomes. As well as quantifiable/physical outcomes (e.g., breastfeeding initiation and duration), Lambert and Loiselle (2007) identified three positive outcomes of health-related information seeking: cognitive, such as increased knowledge and informed decision making; behavioural, including increased self-care abilities and adherence to treatment; and affective, including decreased anxiety, fear, and distress.
Breastfeeding Without Nursing study participants’ outcomes differed based on their information experiences. For example, those who first heard the term exclusive pumping postpartum experienced poorer outcomes. In response to When you first started to exclusive pump, how knowledgeable did you feel about: How to exclusively pump, those who had heard the term exclusive pumping prenatally had a mean score of 46.0 out of 100 (SD = 32.5; n = 338), whereas those who only heard the term postpartum had a mean score of only 27.6 (SD = 29.3; n = 1,069), U = 118,974, z = –9.530, p < .001. This significant difference is not attributable to receiving prenatal breastfeeding education, U = 234,084, z = –0.581, p = .561.
Relatedly, among participants who had completed at least one exclusive pumping journey, there was no significant difference in the duration they exclusively pumped based on whether they had received prenatal or postpartum breastfeeding education. There were, however, significant differences in how knowledgeable participants felt based on whether they had received prenatal and/or postpartum breastfeeding education. Figure 4 illustrates participants’ perception of their knowledge at the beginning of their exclusive pumping journeys about several breastfeeding topics broken down by the amount (none, either prenatal or postpartum, or both) of breastfeeding education they received.
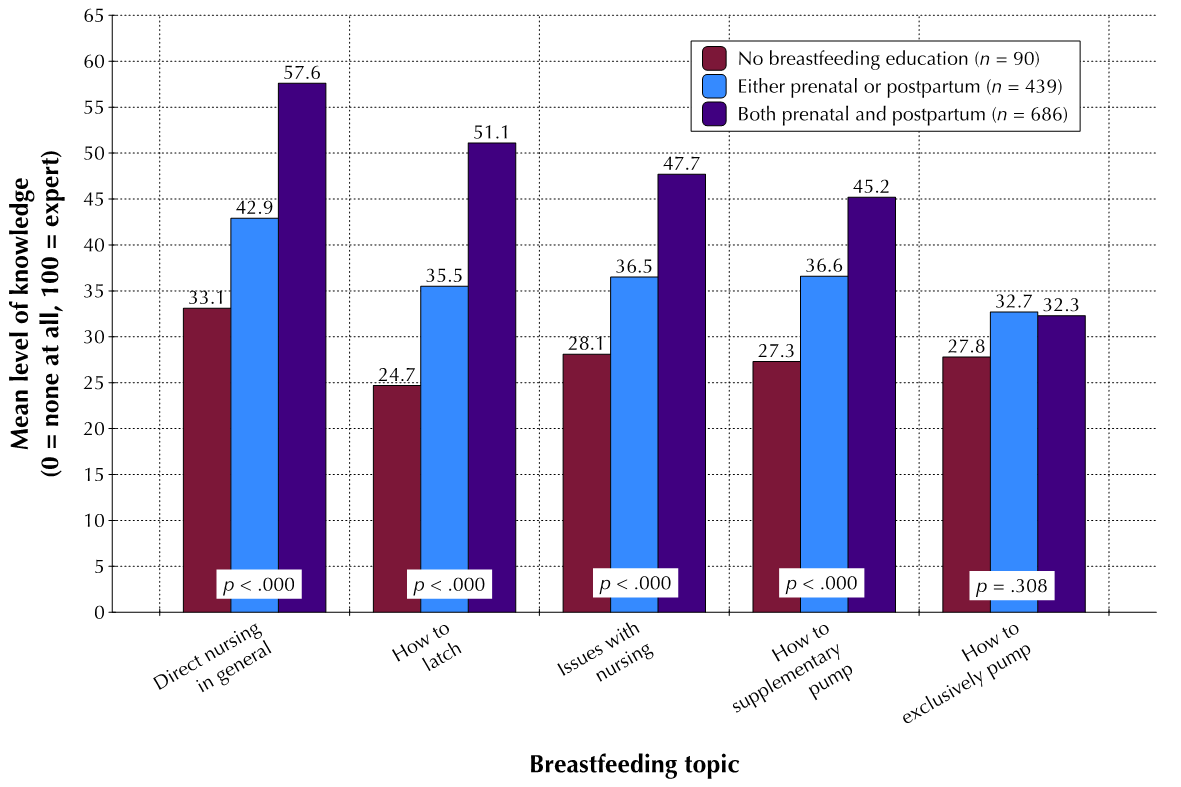
Figure 4. Participants’ perceived level of knowledge when they first started to exclusively pump (n = 1,215)
Notes. Spearman’s rank-order correlations: direct nursing, rs(1,215) = .288; direct nursing problems, rs(1,215) = .311; how to latch, rs(1,215) = .228; how to supplementary pump, rs(1,215) = .185; how to EP, rs(1,215) = 0.029.
For all four questions relating to direct nursing, the amount of participants’ breastfeeding education was associated with significant differences in perceived knowledge. In stark contrast, breastfeeding education made no difference to participants’ perceived knowledge about exclusive pumping which, given that few sources mentioned or explained exclusive pumping (see Figure 2), is not entirely surprising. This participant’s sentiment is representative of many and demonstrates that omission of exclusive pumping information from breastfeeding education has affective consequences:
I even took a breastfeeding class though... Hospital and they barely talked about pumping at all. That was frustrating because regardless of how my breastfeeding journey went I was going back to work so pumping was going to be a reality. They also NEVER mentioned Exclusive Pumping as a thing.
When presented with a list of fifty-six emotions, participants who had only first heard the term exclusive pumping postpartum were more likely to report the emotions listed in Table 4. No emotions were more likely to be reported by participants who first heard the term exclusive pumping prenatally.
| Emotion | Before birth % (n = 321) |
After birth % (n = 1,010) |
χ2 (df = 1, n = 1,331) |
|---|---|---|---|
| Frustrated | 61.1 (196) | 69.5 (702) | 7.916** |
| Abandoned | 4.7 (15) | 8.6 (87) | 5.346* |
| Devoted | 45.8 (147) | 53.1 (536) | 5.160* |
| Rejected | 13.1 (42) | 18.2 (184) | 4.554* |
| Burdened | 43.9 (141) | 50.7 (512) | 4.464* |
| Sad | 34.6 (111) | 41.0 (414) | 4.191* |
| Notes: *p ≤ .05, **p ≤ .01, *** p ≤ .001 | |||
With the exception of feeling devoted, the findings presented in Table 4 suggest that knowing exclusive pumping existed prior to giving birth likely would have improved participants’ affective experiences. Participants who only found out about exclusive pumping postpartum perhaps felt more devoted because they persisted despite these other negative emotions.
Furthermore, those with more breastfeeding education were more likely to report feeling the emotions in Table 5.
| Emotion | p | % selecting this emotion out of participants with that level of education (n) | ||
|---|---|---|---|---|
| No education (n = 94) | Either prenatal or postpartum (n = 492) | Both prenatal and postpartum (n = 784) | ||
| Devoted | 0.001*** | 46.8 (44) | 45.3 (223) | 55.6 (436) |
| Grief | 0.002** | 16.0 (15) | 16.5 (81) | 23.0 (180) |
| Frustrated | 0.006** | 60.6 (57) | 64.2 (316) | 70.5 (553) |
| Resentful | 0.020* | 33.0 (31) | 32.3 (159) | 39.2 (307) |
| Productive | 0.024* | 43.6 (41) | 49.0 (241) | 53.7 (421) |
| Burdened | 0.030* | 36.2 (34) | 48.8 (240) | 50.6 (397) |
| Inadequate | 0.042* | 40.4 (38) | 41.1 (202) | 46.8 (367) |
| Notes: *p ≤ 0.05, **p ≤ 0.01, *** p ≤ 0.001 | ||||
Given that these are predominantly negative, explanations for these associations warrant further investigation since most (93.3%; 1,518/1,627) participants received at least some breastfeeding education. Possible avenues of exploration could include whether overly optimistic breastfeeding information, already known to be detrimental to breastfeeders’ affective outcomes (e.g., Fox et al., 2015), creates unrealistic expectations of direct nursing success, as well as resentment and envy of those that were able to successfully do so. Perhaps the lack of practical and realistic problem-solving information may be behind increased feelings of frustration.
When information sources do not provide exclusive pumpers with the information they need, participants perceived a lack of help and support. When one participant ‘reached out to multiple LCs [lactation consultants] and didn’t get any support with pumping,’ they said that ‘it would have been so easy to give up.’ Lack of information caused participants to lack confidence and experience negative emotions. For example,
If I had known from the beginning that EPing [exclusive pumping] was even a THING then I might have been more confident in my choice earlier on. Also, if I had known that there was no difference in breast milk, whether it comes from a bottle or breast, then I wouldn't have felt so bad.
Some participants even felt they carried the burden of educating their own healthcare providers:
I felt I had to educate my own doctor when I needed the doctor to educate me.
Previous poor experience with information sources also had measurable quantitative outcomes. For example, a Cochran-Armitage test of trend showed a statistically significant linear trend (p < .001) between how useful a participant rated the exclusive pumping information they received from a lactation consultant and whether they sought help from a medical professional if they had a breast health problem related to exclusive pumping. While 49.9% (168/337) of those that rated exclusive pumping information from a lactation consultant as very useful sought medical help for a breast/nipple health problem, only 33.7% (86/225) of those rating lactation consultant information as not at all useful sought this help. It is concerning to consider that anyone might hesitate to seek medical help because of previous poor information experiences—even more so when lack of medical attention for a breastfeeding-related breast health problem potentially impacts a breastfeeder’s ability to produce milk, feed their baby, and fulfil their breastfeeding intentions. It is critical that this finding is explored more thoroughly.
Information seeking barriers
Barriers to acquiring information are physical, affective, or cognitive ‘obstacles hindering, delaying or preventing access to information, that is, information seeking, searching and using’ (Świgoń, 2011, p. 475). Physical barriers may be ‘spatial (e.g., long distance to a library), temporal (e.g., an absolute deadline limiting the time available for information seeking), or socio-cultural (e.g., bureaucratic inertia)’ (Savolainen, 2016, p. 52). Affective barriers may be associated with information avoidance, whereas cognitive barriers may relate to a lack of literacy or poor search skills.
With increased reliance on non-mediated information seeking (i.e., without the assistance of someone else, like a subject expert or information professional), such as looking on the internet, knowing the name of the thing you are looking for becomes even more essential (see, for example, Furnas et al., 1987). Active seeking, or even scanning, for information becomes difficult when an individual does not know what it is they are looking for. Many Breastfeeding Without Nursing study participants had no choice but to search for other terms, until they serendipitously came across exclusive pumping. For example:
I didn’t learn about exclusive pumping until I was 4 months postpartum with my first. Mainly because I didn’t know it was an actual thing and didn’t know what to call it. My supply had dropped to nothing because I had no education on how to keep it going. Through random Google searches I finally found some websites and I was able to get lots of information.
Conflicting information creates a barrier to successful breastfeeding and may lead to trust issues, deference to the source people deem (potentially incorrectly) most credible, and negative affective outcomes (Carpenter et al., 2016). Mothers in Fox et al.’s (2015) study reported that breastfeeding ‘advice was often inadequate, contradictory and undermined their confidence in their feeding abilities’ (p. 152). In their answers to What unanswered questions do you still have about EPing? Where have you looked for answers?, many Breastfeeding Without Nursing study participants commented that their unanswered questions pertained to issues on questions to which they have received conflicting answers. For example:
How long can breast milk be left out at room temperature, in the refrigerator, in the freezer, and in a deep freezer? I have looked online and in the Facebook groups I am a member of and get mixed answers.
Some participants struggled with specific sources that conflicted with one another:
Been trying to find the information [about pumping schedules] on online forums but there seems to be conflicting reports so it’s very confusing.
Encountering misinformation, either actual or perceived, was also a barrier to information seeking for some participants:
I learned through trial and error and from sources on the Internet. Some of the answers were helpful. Others were hard to find accurate info. The sources of info could be rife with misinformation… their reliability could and should be called in to question. You really needed to check the validity of the info received, and that was hard in a lot of cases.
When information is confusing, overwhelming, incomplete, or wrong, it can also cause anxiety, as well as be a burden and lead to information avoidance (Crook et al., 2016). When cognitive effort must be made to try to make sense of information, cognitive biases are exacerbated and errors in judgment increase (Carpenter et al., 2016). For example:
There’s a LOT of information on the internet and sometimes its conflicting so it’s hard to know what’s right/wrong especially when you’re a first time mom.
Online sources made me a bit more anxious than talking to my friend as there was just too much info to sift through. My friend felt like an expert, distilling all of the info based on her experiences. That helped immensely!
Judgement by others is another barrier to seeking and receiving information. Loudon et al. (2016) found that, even online, ‘mothers feared being ‘judged’ by other mothers, family, and HCPs about their parenting choices, causing them to hold back and refrain from seeking advice on contentious or sensitive topics in particular’ (p. 39). Breastfeeding Without Nursing study participants expressed feeling judged from a variety of sources. For example:
I felt very judged by the nurses caring for my son in the nursery after birth. They wouldn’t call me down for feedings as promised and provided contradicting advice on how/when to nurse. … I finally saw a lactation consultant who was not helpful at all and I felt further judged by her.
I think what has been most important to me in these [online support] groups has been the support provided, given in a non-judgmental way no matter how they were feeding, whether they were EPing [exclusively pumping], supplementing, combo pumping and nursing, or deciding to wean to formula.
I do agree that breastfeeding or exclusively pumping is a great way to figure child but I also do not find anything wrong with providing your child with an alternate source, but today’s society is so judgmental and so demeaning that your almost bullied into no other option.
It is against this backdrop that these breastfeeders would have to reach out for support, clearly a daunting task if they feared or had already experienced the judgment of others for their breastfeeding without nursing.
So-called experts but who have poor subject knowledge also create a barrier to seeking breastfeeding, and especially pumping, information. Doctors receive little-to-no lactation education (Osband et al., 2011) and it is unclear what amount of pumping education lactation consultants receive. From personal experience I can report that, as part of the 45-hour Certified Lactation Counselor course, I only recall approximately 30 minutes dedicated to milk expression. No formal qualification or certification exists to demonstrate knowledge of milk expression, despite the ubiquity of the practice. More information was the number one theme identified in participants’ answers to What would have made your experience of EPing better?; participants often added that this information should have come from a lactation consultant. Some participants even taught their own healthcare providers about exclusive pumping. For example:
I was teaching my OB [obstetrician] and my Pediatrician about what I was doing -- they were both very supportive but relatively uneducated about the topic [exclusive pumping].
Lastly, there is a lack of empirical data about most aspects of exclusive pumping. Several participants commented on this lack. For example:
There doesn’t seem to be a lot of research or empirical data on increasing your supply while EPing [exclusive pumping]. Much of it appears to be anecdotal at best or apply solely to those that only pump for supplemental feeding purposes.
There needs to be more research into it scientifically. I’m sick of guessing. There needs to be more information and presented as an option.
This lack of data is problematic, especially for evidence-based practitioners such as lactation consultants who may find it challenging to make recommendations based on anecdotal evidence. Consequently, they may make little-to-no recommendations or share only scant information about exclusive pumping, leaving breastfeeders who need this information support bereft.
Conclusion
Exclusive pumpers’ information experience is characterised by a profound lack of information from lactation consultants and a perception of high-quality information and support from online sources, especially online support groups. Granted, recruitment for this study was conducted predominantly through these very same sites, but overwhelmingly, participants only joined these groups after birth having already experienced an exclusive pumping information desert. These—predominantly White, Unites States resident, relatively well-off, and well-educated—participants were lucky to have the ability (digital, physical, intellectual, etc.) to discover an oasis of information and become part of rich online communities; it is impossible to ever discover how many breastfeeders (or want-to-bes) are excluded from experiencing exclusive pumping information in this way. There is, therefore, a critical need for all healthcare providers, but especially lactation consultants to provide timely practical, informational, and emotional support, especially in light of the poor information experiences with lactation consultants endured by many of the participants in this study.
Findings from this study have a number of implications for those providing lactation care, namely lactation consultants. Until formal education and resources on exclusive pumping are developed, lactation consultants have a duty to utilise the resources that are available to learn about exclusive pumping. Taking online courses and reading blogs, websites, and the few books that are available, although directed at breastfeeders and not lactation consultants, still provide useful information. These activities would also better prepare lactation consultants to counsel and advise exclusive pumpers, given that they would have insight into their information needs and any potential misinformation or concerning practices being propagated within the exclusive pumping community. Following the social media accounts of pump and accessory manufacturers, as well as social media influencers, again provides information about the products available and advice/information being widely distributed. While recommending commercial products risks a conflict of interest, especially in light of lactation consultants’ codes of ethics, at the very least discussing them is unavoidable if lactation consultants are to provide comprehensive, high quality care to their pumping clients.
Future work in this area could take several different courses. That information about exclusive pumping on online support groups was of far higher perceived quality, in both quantity and accuracy, than expert sources is a novel and disruptive finding, especially in light of the current proliferation of fake news on social networking sites. Multiple questions arise from this finding. For example, given the quasi-medical nature of breastfeeding information, what are the risks of receiving information from potentially untrained sources? Is this finding unique to this specific topic or does it exist in other consumer health or everyday life information seeking situations? If social media has become the preferred source of information about certain topics, what effect does this have on the perception of information from other sources? How are those who do not or cannot participate on social networking sites affected?
By examining the information experience faced by exclusive pumpers and identifying the gaps in exclusive pumping information, the support that exclusive pumpers need and deserve, but seldom receive enough of, can be vastly improved. In an ideal world, all breastfeeders should be able to fully fulfil their original breastfeeding intentions and goals, but for a variety of reasons, this is just not a realistic outcome. When exclusive pumping becomes the only way a breastfeeder can feed their child, it is vital that all those who support breastfeeding, but especially lactation consultants, provide practical, informational, and emotional support of the highest quality to prevent the double let down of nursing failure together with poor lactation support for the only alternative that still enables these breastfeeders to feed their own milk to their child.
Acknowledgements
I am forever grateful for the time and vulnerability given so generously by the Breastfeeding Without Nursing study participants. My PhD advisor, Dr. Beth St. Jean, has been a constant support and I greatly appreciate her thorough and insightful comments on my research and writing. I deeply appreciate the comments of the peer reviewers, which not only shaped the revisions to this paper, but the reframing of this topic within my PhD dissertation.
About the author
Fiona M. Jardine earned her PhD in Information Studies in May 2020 from the College of Information Studies, University of Maryland, College Park, Maryland, 20742, USA. Her research interests include how socioecological factors influence information experience and the effect on individual and population health outcomes. She can be reached at fjardine@umd.edu.
References
- American Academy of Pediatrics. (2012). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. https://doi.org/10.1542/peds.2011-3552
- Angell, C. (2017). An everyday trauma: How the media portrays infant feeding. In L. Ann, V. Hundley, & E. van Teijlingen (Eds.), Midwifery, Childbirth and the Media (Vol. 28, Issue 3, pp. 45–59). Palgrave Macmillan. https://doi.org/10.1007/978-3-319-63513-2_4
- Asiodu, I. V., Waters, C. M., Dailey, D. E., Lee, K. A., & Lyndon, A. (2015). Breastfeeding and use of social media among first-time African American mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(2), 268–278. https://doi.org/10.1111/1552-6909.12552
- Bai, D. L., Fong, D. Y. T., Lok, K. Y. W., Wong, J. Y. H., & Tarrant, M. (2017). Practices, predictors and consequences of expressed breast-milk feeding in healthy full-term infants. Public Health Nutrition, 20(3), 492–503. https://doi.org/10.1017/S136898001600241X
- Bartholomew, M. K., Schoppe-Sullivan, S. J., Glassman, M., Kamp Dush, C. M., & Sullivan, J. M. (2012). New parents’ Facebook use at the transition to parenthood. Family Relations, 61(3), 455–469. https://doi.org/10.1111/j.1741-3729.2012.00708.x
- Bartick, M. C., & Reinhold, A. G. (2010). The burden of suboptimal breastfeeding in the United States: A pediatric cost analysis. Pediatrics, 125(5). https://doi.org/10.1542/peds.2009-1616
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Brown, A. (2016). What do women really want? Lessons for breastfeeding promotion and education. Breastfeeding Medicine, 11(3), 102–110. https://doi.org/10.1089/bfm.2015.0175
- Brown, A. (2019). Why breastfeeding grief and trauma matter (Pinter & Martin Why It Matters 17). Pinter & Martin.
- Bruce, C., Davis, K., Hughes, H., Partridge, H., & Stoodley, I. (2014a). Information Experience: Contemporary Perspectives. In Information Experience: Approaches to Theory and Practice (Vol. 9, pp. 3–15). https://doi.org/10.1108/S1876-056220140000010001
- Bruce, C., Davis, K., Hughes, H., Partridge, H., & Stoodley, I. (2014b). Information experience: New perspectives and research directions. In Information Experience: Approaches to Theory and Practice (pp. 315–320). https://doi.org/10.1108/S1876-056220140000010016
- Bruce, H. (2005). Personal, anticipated information need. Information Research, 10(3).
- Carpenter, D. M., Geryk, L. L., Chen, A. T., Nagler, R. H., Dieckmann, N. F., & Han, P. K. J. (2016). Conflicting health information: A critical research need. Health Expectations, 19(6), 1173–1182. https://doi.org/10.1111/hex.12438
- Case, D. O., Andrews, J. E., Johnson, J. D., & Allard, S. L. (2005). Avoiding versus seeking: The relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. Journal of the Medical Library Association, 93(3), 353–362.
- Case, D. O., & Given, L. M. (2016). Looking for information: A survey of research on information seeking, needs, and behavior (4th ed.). Emerald Publishing Group.
- Clifford, J., & McIntyre, E. (2008). Who supports breastfeeding? Breastfeeding Review: Professional Publication of the Nursing Mothers’ Association of Australia, 16(2), 9–19.
- Colen, C. G., & Ramey, D. M. (2014). Is breast truly best? Estimating the effects of breastfeeding on long-term child health and wellbeing in the United States using sibling comparisons. Social Science & Medicine, 109, 55–65. https://doi.org/10.1016/j.socscimed.2014.01.027
- Cox, K., Giglia, R., & Binns, C. W. (2017). Breastfeeding beyond the big smoke: Who provides support for mothers in rural Western Australia? Australian Journal of Rural Health, 25(6), 369–375. https://doi.org/10.1111/ajr.12362
- Crook, B., Stephens, K. K., Pastorek, A. E., Mackert, M., & Donovan, E. E. (2016). Sharing health information and influencing behavioral intentions: The role of health literacy, information overload, and the internet in the diffusion of healthy heart information. Health Communication, 31(1), 60–71. https://doi.org/10.1080/10410236.2014.936336
- De Choudhury, M., Counts, S., & Horvitz, E. (2013). Major life changes and behavioral markers in social media: Case of childbirth. Proceedings of the ACM Conference on Computer Supported Cooperative Work, CSCW, 13, 1431–1442. https://doi.org/10.1145/2441776.2441937
- Dennis, C.-L., & McQueen, K. (2007). Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatrica, 96(4), 590–594. https://doi.org/10.1111/j.1651-2227.2007.00184.x
- Dietrich Leurer, M., McCabe, J., Bigalky, J., Mackey, A., Laczko, D., & Deobald, V. (2019). “We just kind of had to figure it out”: A qualitative exploration of the information needs of mothers who express human milk. Journal of Human Lactation, PG-890334419883203, 1–10. https://doi.org/10.1177/0890334419883203
- Dietrich Leurer, M., & Misskey, E. (2015). “Be positive as well as realistic”: A qualitative description analysis of information gaps experienced by breastfeeding mothers. International Breastfeeding Journal, 10(10), 1–11. https://doi.org/10.1186/s13006-015-0036-7
- Erdelez, S. (1997). Information encountering: A conceptual framework for accidental information discovery. ISIC ’96 Proceedings of an International Conference on Information Seeking in Context, December, 412–421.
- Erdelez, S., Heinström, J., Makri, S., Björneborn, L., Beheshti, J., Toms, E., & Agarwal, N. K. (2016). Research perspectives on serendipity and information encountering. Proceedings of the Association for Information Science and Technology, 53(1), 1–5. https://doi.org/10.1002/pra2.2016.14505301011
- Felice, J. P., & Rasmussen, K. M. (2015). Breasts, pumps and bottles, and unanswered questions. Breastfeeding Medicine, 10(9), 412–415. https://doi.org/10.1089/bfm.2015.0107
- Fox, R., McMullen, S., & Newburn, M. (2015). UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of Baby Café services. BMC Pregnancy and Childbirth, 15(147), 1–12. https://doi.org/10.1186/s12884-015-0581-5
- Fu, I. C. Y., Fong, D. Y. T., Heys, M., Lee, I. L. Y., Sham, A., & Tarrant, M. (2014). Professional breastfeeding support for first-time mothers: A multicentre cluster randomised controlled trial. BJOG: An International Journal of Obstetrics and Gynaecology, 121(13), 1673–1683. https://doi.org/10.1111/1471-0528.12884
- Furnas, G. W., Landauer, T. K., Gomez, L. M., & Dumais, S. T. (1987). The vocabulary problem in human-system communication. Communications of the ACM, 30(11), 964–971. https://doi.org/10.1145/32206.32212
- Graffy, J., & Taylor, J. L. (2005). What information, advice, and support do women want with breastfeeding? Birth, 32(3), 179 186. https://doi.org/10.1111/j.0730-7659.2005.00367.x
- Gray, J. (2013). Feeding on the web: Online social support in the breastfeeding context. Communication Research Reports, 30(1), 1–11. https://doi.org/10.1080/08824096.2012.746219
- Grimes, H. A., Forster, D. A., & Newton, M. S. (2014). Sources of information used by women during pregnancy to meet their information needs. Midwifery, 30(1), e26–e33. https://doi.org/10.1016/j.midw.2013.10.007
- Hauck, Y. L., & Irurita, V. (2003). Incompatible expectations: The dilemma of breastfeeding mothers. Health Care for Women International, 24(1), 62–78. https://doi.org/10.1080/07399330304023
- Hegney, D., Fallon, T., & O’Brien, M. L. (2008). Against all odds: A retrospective case-controlled study of women who experienced extraordinary breastfeeding problems. Journal of Clinical Nursing, 17(9), 1182–1192. https://doi.org/10.1111/j.1365-2702.2008.02300.x
- Hornbeak, D. M., Dirani, M., Sham, W. K., Li, J., Young, T. L., Wong, T. Y., Chong, Y. S., & Saw, S. M. (2010). Emerging trends in breastfeeding practices in Singaporean Chinese women: Findings from a population-based study. Annals of the Academy of Medicine Singapore, 39(2), 88–94. NS -
- Horowitz, J., Parker, K., Graf, N., & Livingston, G. (2017). Americans widely support paid family and medical leave, but differ over specific policies. In Pew Research Center. www.pewresearch.org
- Hoyer, S., & Horvat, L. (2000). Successful breast-feeding as a result of a health education programme for mothers. Journal of Advanced Nursing, 32(5), 1158–1167. https://doi.org/10.1046/j.1365-2648.2000.01553.x
- Jardine, F. M. (2020). Use of language in "When online support groups prevail: the information experience of chest/breastfeeders who only express their milk" for ISIC 2020. https://fionamjardine.com/isic2020/
- Jardine, F. M. (2018). Breastfeeding without nursing: Reasons for initiation and cessation of exclusively pumping human milk: Abstracts from the 19th International Society for Research in Human Milk and Lactation Conference. Breastfeeding Medicine, 13(7), A-43. https://doi.org/10.1089/bfm.2018.29100.abstracts
- Kamali, S., Ahmadian, L., Khajouei, R., & Bahaadinbeigy, K. (2018). Health information needs of pregnant women: Information sources, motives and barriers. Health Information and Libraries Journal, 35(1), 24–37. https://doi.org/10.1111/hir.12200
- Karmacharya, C., Cunningham, K., Choufani, J., & Kadiyala, S. (2017). Grandmothers’ knowledge positively influences maternal knowledge and infant and young child feeding practices. Public Health Nutrition, 20(12), 2114–2123. https://doi.org/10.1017/S1368980017000969
- Kukla, R., & Wayne, K. (2016). Pregnancy, birth, and medicine. The Stanford Encyclopedia of Philosophy. https://plato.stanford.edu/archives/spr2018/entries/ethics-pregnancy/
- Labbok, M. H. (2008). Transdisciplinary breastfeeding support: Creating program and policy synergy across the reproductive continuum. International Breastfeeding Journal, 3(1), 16. https://doi.org/10.1186/1746-4358-3-16
- Labiner-Wolfe, J., Fein, S. B., Shealy, K. R., & Wang, C. (2008). Prevalence of breast milk expression and associated factors. Pediatrics, 122(Supplement 2), S63–S68. https://doi.org/10.1542/peds.2008-1315h
- Lambert, S. D., & Loiselle, C. G. (2007). Health information-seeking behavior. Qualitative Health Research, 17(8), 1006–1019. https://doi.org/10.1177/1049732307305199
- Lee, E. (2008). Living with risk in the age of “intensive motherhood”: Maternal identity and infant feeding. Health, Risk and Society, 10(5), 467–477. https://doi.org/10.1080/13698570802383432
- Li, R., Perrine, C. G., Anstey, E. H., Chen, J., MacGowan, C. A., & Elam-Evans, L. D. (2019). Breastfeeding trends by race/ethnicity among US children born from 2009 to 2015. JAMA Pediatrics, 173(12), e193319. https://doi.org/10.1001/jamapediatrics.2019.3319
- Loudon, K., Buchanan, S., & Ruthven, I. (2016). The everyday life information seeking behaviours of first-time mothers. Journal of Documentation, 72(1), 24–46. https://doi.org/10.1108/JD-06-2014-0080
- Lumbiganon, P., Martis, R., Laopaiboon, M., Festin, M. R., Ho, J. J., & Hakimi, M. (2016). Antenatal breastfeeding education for increasing breastfeeding duration. Cochrane Database of Systematic Reviews, 12, CD006425. https://doi.org/10.1002/14651858.CD006425.pub4
- Madge, C., O’Connor, H., Connor, H. O., Madge, C., & Connor, H. O. (2006). Parenting gone wired: Empowerment of new mothers on the internet? Social & Cultural Geography, 7(2), 199–220. https://doi.org/10.1080/14649360600600528
- McDougall, R., & Ecclestone, K. (2015). Information seeking during pregnancy: Exploring the changing landscape and planning for the future. In Wellington-Dufferin-Guelph Public Health. https://www.wdgpublichealth.ca/sites/default/files/file-attachments/report/ht_report_2015-information-seeking-during-pregnancy_access.pdf
- McInnes, R. J., Arbuckle, A., & Hoddinott, P. (2015). How UK internet websites portray breast milk expression and breast pumps: A qualitative study of content. BMC Pregnancy and Childbirth, 15(1), 1–11. https://doi.org/10.1186/s12884-015-0509-0
- McKeever, R., & McKeever, B. W. (2017). Moms and media: Exploring the effects of online communication on infant feeding practices. Health Communication, 32(9), 1059–1065. https://doi.org/10.1080/10410236.2016.1196638
- McKenzie, P. J. (2003). A model of information practices in accounts of everyday‐life information seeking. Journal of Documentation, 59(1), 19–40. https://doi.org/10.1108/00220410310457993
- Moses, Y. (2016). Is the term “people of color” acceptable in this day and age? Sapiens: Anthropology/Everything Human. https://www.sapiens.org/column/race/people-of-color/
- Mozingo, J. N., Davis, M. W., Droppleman, P. G., & Merideth, A. (2000). “It wasn’t working”: Women’s experiences with short-term breastfeeding. The American Journal of Maternal/Child Nursing, 25(3), 120.
- Nolan, S., Hendricks, J., Ferguson, S., & Towell, A. (2017). Social networking site (SNS) use by adolescent mothers: Can social support and social capital be enhanced by online social networks? – A structured review of the literature. In Midwifery (Vol. 48, Issue March, pp. 24–31). Elsevier Ltd. https://doi.org/10.1016/j.midw.2017.03.002
- Osband, Y. B., Altman, R. L., Patrick, P. A., & Edwards, K. S. (2011). Breastfeeding education and support services offered to pediatric residents in the US. Academic Pediatrics, 11(1), 75–79. https://doi.org/10.1016/j.acap.2010.11.002
- Papen, U. (2013). Conceptualising information literacy as social practice: A study of pregnant women’s information practices. Information Research, 18(2). http://www.informationr.net/ir/18-2/paper580.html#.XlCg5C2ZN5M
- Rasmussen, K. M., & Geraghty, S. R. (2011). The quiet revolution: Breastfeeding transformed with the use of breast pumps. American Journal of Public Health, 101(8), 1356–1359. https://doi.org/10.2105/AJPH.2011.300136
- Rood, J. A. J., Van Zuuren, F. J., Stam, F., van der Ploeg, T., Huijgens, P. C., & Verdonck- de Leeuw, I. M. (2015). Cognitive coping style (monitoring and blunting) and the need for information, information satisfaction and shared decision making among patients with haematological malignancies. Psycho-Oncology, 24(5), 564–571. https://doi.org/10.1002/pon.3699
- Savolainen, R. (2009). Everyday life information seeking. In M. J. Bates & M. N. Maack (Eds.), Encyclopedia of Library and Information Sciences (3rd Editio, pp. 1780–1789). CRC Press. https://doi.org/10.1081/E-ELIS3-120043920
- Savolainen, R. (2016). Approaches to socio-cultural barriers to information seeking. Library and Information Science Research, 38(1), 52–59. https://doi.org/10.1016/j.lisr.2016.01.007
- Savolainen, R. (2019). Elaborating the sensory and cognitive-affective aspects of information experience. Journal of Librarianship and Information Science, 1–14. https://doi.org/10.1177/0961000619871595
- Sayakhot, P., & Carolan-Olah, M. (2016). Internet use by pregnant women seeking pregnancy-related information: A systematic review. BMC Pregnancy and Childbirth, 16(65), 1–10. https://doi.org/10.1186/s12884-016-0856-5
- Shakya, P., Kunieda, M. K., Koyama, M., Rai, S. S., Miyaguchi, M., Dhakal, S., Sandy, S., Sunguya, B. F., & Jimba, M. (2017). Effectiveness of community-based peer support for mothers to improve their breastfeeding practices: A systematic review and meta-analysis. PLoS ONE, 12(5), e0177434:1-24. https://doi.org/10.1371/journal.pone.0177434
- Smale, M., Renfrew, M. J., Marshall, J. L., & Spiby, H. (2006). Turning policy into practice: More difficult than it seems. The case of breastfeeding education. Maternal and Child Nutrition, 2(2), 103–113. https://doi.org/10.1111/j.1740-8709.2006.00045.x
- Song, H., Cramer, E. M., McRoy, S., & May, A. (2013). Information needs, seeking behaviors, and support among low-income expectant women. Women and Health, 53(8), 824–842. https://doi.org/10.1080/03630242.2013.831019
- Spear, H. J. (2004). When reality does not meet expectations: The importance of consistent communication, support, and anticipatory guidance for high-risk mothers who plan to breastfeed. Journal of Clinical Nursing, 13(6), 773–775. https://doi.org/10.1111/j.1365-2702.2004.00956.x
- Spiro, A. (2016). Why do so many breastfeeding mothers stop before they want to? Journal of Health Visiting, 4(3), 126–128. https://doi.org/10.12968/johv.2016.4.3.126
- Sutter, C., Fiese, B. H., Lundquist, A., Davis, E. C., McBride, B. A., & Donovan, S. M. (2018). Sources of information and support for breastfeeding: Alignment with Centers for Disease Control and Prevention strategies. Breastfeeding Medicine, 13(9), 598–606. https://doi.org/10.1089/bfm.2018.0056
- Świgoń, M. (2011). Information barriers in libraries: Types, typologies and Polish empirical studies. Library Management, 32(6), 475–484. https://doi.org/10.1108/01435121111158619
- Thomson, G., Ebisch-Burton, K., & Flacking, R. (2015). Shame if you do - shame if you don’t: Women’s experiences of infant feeding. Maternal and Child Nutrition, 11(1), 33–46. https://doi.org/10.1111/mcn.12148
- Victora, C. G., Bahl, R., Barros, A. J. D., França, G. V. A., Horton, S., Krasevec, J., Murch, S., Sankar, M. J., Walker, N., Rollins, N. C., Allen, K., Dharmage, S., Lodge, C., Peres, K. G., Bhandari, N., Chowdhury, R., Sinha, B., Taneja, S., Giugliani, E., … Richter, L. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. In The Lancet (Vol. 387, Issue 10017, pp. 475–490). https://doi.org/10.1016/S0140-6736(15)01024-7
- Von Glasersfeld, E., & Ackermann, E. K. (2011). Reflections on the concept of experience and the role of consciousness: Unfinished fragments. Constructivist Foundations, 6(2), 193–203.
- World Health Organization. (2003). Global strategy for infant and young child feeding. World Health Organization.
- Williamson, I., Leeming, D., Lyttle, S., & Johnson, S. (2012). “It should be the most natural thing in the world”: Exploring first-time mothers’ breastfeeding difficulties in the UK using audio-diaries and interviews. Maternal and Child Nutrition, 8(4), 434–447. https://doi.org/10.1111/j.1740-8709.2011.00328.x
- Williamson, K. (1998). Discovered by chance: The role of incidental information acquisition in an ecological model of information use. Library and Information Science Research, 20(1), 23–40. https://doi.org/10.1016/S0740-8188(98)90004-4
- Wilson, T. D. (2000). Human information behavior. Informing Science: The International Journal of an Emerging Transdiscipline, 3(2), 49–56. https://doi.org/10.28945/576
- Yamada, R., Rasmussen, K. M., & Felice, J. P. (2016). Mothers’ use of social media to inform their practices for pumping and providing pumped human milk to their infants. Children, 3(4), 22:1-12. https://doi.org/10.3390/children3040022
- Zimmerman, D. H., & Wieder, D. L. (1977). The diary: Diary-interview method. Journal of Contemporary Ethnography, 5(4), 479–498. https://doi.org/10.1177/089124167700500406